FAQs for NDIS Providers - Managing Reportable Incidents
Under the NDIS Quality and Safeguarding Framework, all registered NDIS providers must follow strict procedures for identifying, responding to, and reporting serious incidents. These are known as Reportable Incidents, and managing them correctly is essential for participant safety, provider compliance, and maintaining NDIS registration.
Below is a detailed FAQ to help providers understand their responsibilities and respond effectively.
What is a Reportable Incident under the NDIS?
A Reportable Incident is a serious incident that occurs, or is alleged to have occurred, in connection with NDIS support or services. Registered providers are legally required to notify the NDIS Quality and Safeguards Commission when these incidents occur.
Only specific types of incidents are considered “reportable,” and they must meet defined criteria.
What types of incidents must be reported to the NDIS Commission?
The following are classified as Reportable Incidents:

- The death of a participant
- Serious injury of a participant
- Abuse or neglect of a participant
- Unlawful physical contact or assault
- Sexual misconduct, including grooming or sexual assault
- Unauthorised Restrictive Practices (use, attempted use, or misuse)
Even if the provider only becomes aware of the allegation later, it must still be reported.
What is the timeframe for reporting a Reportable Incident?
Providers must notify the NDIS Commission within 24 hours of becoming aware of:
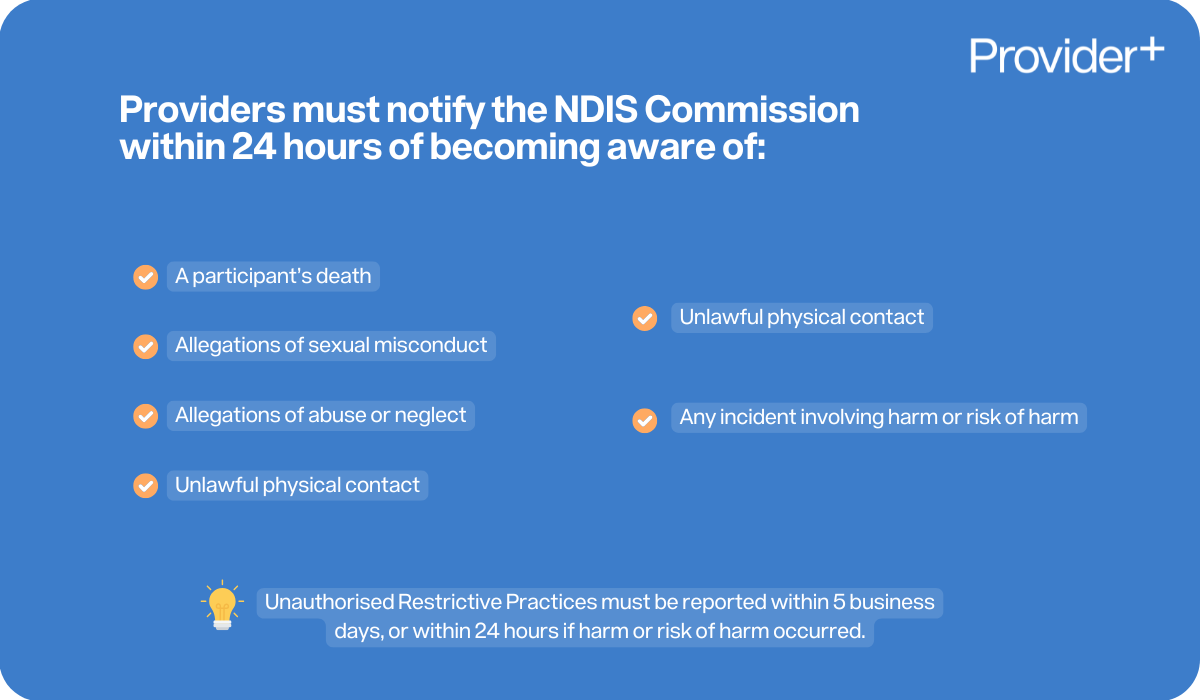
- A participant’s death
- Allegations of sexual misconduct
- Allegations of abuse or neglect
- Serious injury
- Unlawful physical contact
- Any incident involving harm or risk of harm
Unauthorised Restrictive Practices must be notified within 5 business days, unless the incident caused harm or risk of harm, in which case it must be reported within 24 hours.
How do I report a Reportable Incident to the NDIS Commission?
- Log in to the NDIS Commission Portal
- Go to “My Reportable Incidents”
- Complete and submit the following forms:
- Immediate Notification Form
- 5 Day Form
Do providers have to submit a follow-up report?
Yes. After the initial 24 hour notification, a follow-up report is required within 5 business days. This report must include:
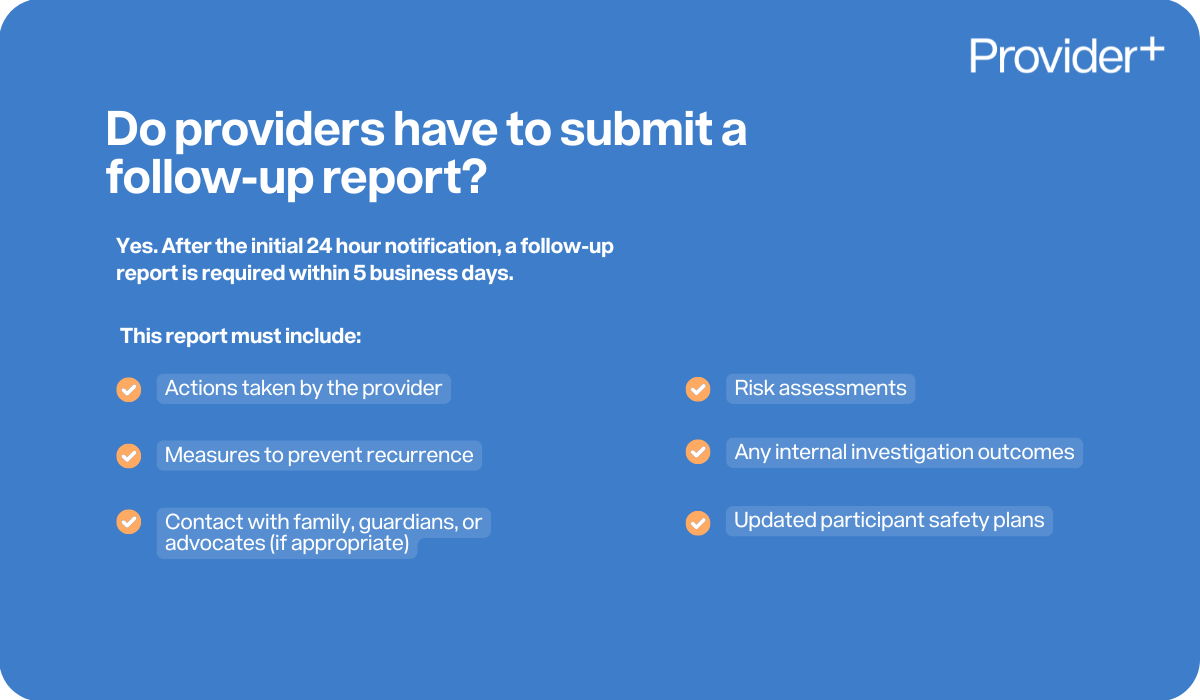
- Actions taken by the provider
- Measures to prevent recurrence
- Contact with family, guardians, or advocates (if appropriate)
- Risk assessments
- Any internal investigation outcomes
- Updated participant safety plans
The Commission may request further updates, depending on the seriousness of the incident.
Do all incidents need to be reported?
No. Only the specific categories of Reportable Incidents must be notified to the NDIS Commission.
However, all other incidents including minor injuries, behavioural changes, medication errors, or environmental hazards still need to be:
- Recorded internally within an incident report and incident register
- Reviewed by management and
- Managed through the provider’s incident management system
These internal incidents help identify trends, reduce risk, and demonstrate continuous improvement.
What is an Unauthorised Restrictive Practice?
A restrictive practice is any practice that restricts a person’s rights, freedom, or movement.
Examples include:

- Chemical restraint
- Physical restraint
- Mechanical restraint
- Seclusion
- Environmental restraint
An unauthorised restrictive practice occurs when:
- There is no approved Behaviour Support Plan
- There is no authorisation under state/territory laws
- The practice is used incorrectly or without consent
All unauthorised restrictive practices must be reported to the NDIS Quality & Safeguards Commission within 5 business days.
What should support workers do when an incident occurs?
Support workers have a duty of care to respond immediately. They must:

- Ensure the participant is safe
- Call emergency services if required
- Notify their supervisor or manager as soon as possible
- Record factual details in the incident management system
- Cooperate fully with documentation, investigations, or reviews
Who is responsible for reporting the incident to the NDIS Commission?
The responsibility lies with the authorised reporting delegate within the registered NDIS provider, not the individual worker involved in the incident. The worker does play a crucial role in reporting the incident internally so the provider and its reporting delegate can take the next steps.
Do providers have to notify the participant’s family or guardian?
Yes. Providers must ensure that family members, guardians, nominees, or key decision-makers are notified unless the participant requests otherwise or it is not appropriate due to legal or safeguarding reasons. Participant choice, control and privacy should always be respected.
What happens after a Reportable Incident is lodged?
Once the NDIS Commission receives the notification, they may:
- Request further information
- Monitor the provider’s response
- Require an internal investigation
- Conduct their own investigation
- Provide directions to improve systems
- Review the provider’s compliance history
The provider must demonstrate effective incident management, corrective action, and risk reduction strategies.
What is the purpose of reporting incidents?
The goal is not to scrutinise or penalise providers unnecessarily, but to:

- Keep participants safe
- Identify systemic risks
- Ensure providers take corrective action
- Improve service quality
- Strengthen safeguarding
- Prevent recurring harm
Regular reporting fosters a culture of transparency and continuous improvement.
What if a provider does not report a required incident?
Failing to report can be viewed as a breach of participant safety obligations. Serious consequences can apply, including:
- Regulatory action
- Compliance notices
- Penalties
- Conditions placed on registration
- Cancellation of registration
What documentation should providers keep?
Providers should maintain:
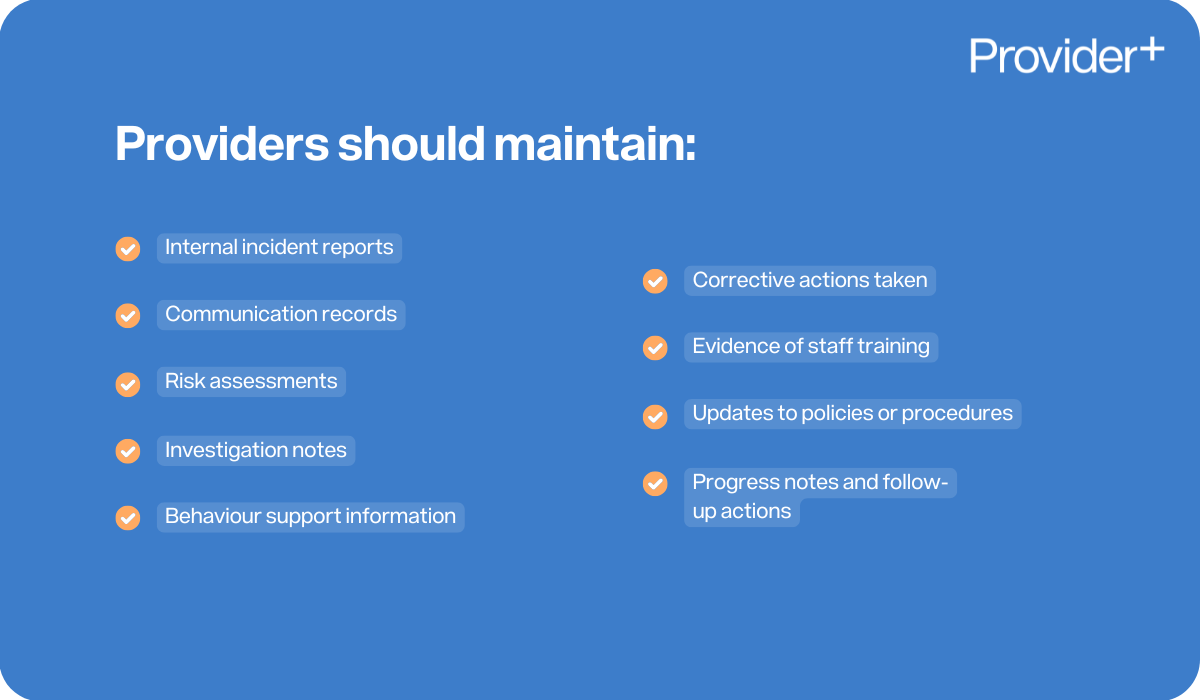
- Internal incident reports
- Communication records
- Risk assessments
- Investigation notes
- Behaviour support information
- Corrective actions taken
- Evidence of staff training
- Updates to policies or procedures
- Progress notes and follow-up actions
These records must be complete, factual, and securely stored.
How can providers reduce the risk of incidents?
Implementing a proactive approach helps minimise future harm. Preventative strategies include:
- Thorough staff training
- Clear participant profiles and risk assessments
- Strong behaviour support planning
- Regular environmental and safety checks
- Clear escalation protocols
- Transparent & strong communication with families and allied health professionals
- Reviewing incident patterns to identify trends
Do staff need training in Reportable Incident management?
Yes, conducting training on Reportable Incident Management is a requirement of the NDIS Practice Standards which requires for workers to understand:
- What a Reportable Incident is
- How to identify incidents
- How to respond to emergencies
- The provider’s internal incident management system
- Their legal and ethical responsibilities
Training must be ongoing, documented, and refreshed regularly.
Conclusion
Managing Reportable Incidents under the NDIS is an essential part of keeping participants safe and maintaining high-quality service delivery. Understanding the reporting requirements, maintaining transparency, and responding quickly can significantly reduce risk and improve outcomes for participants.
A strong incident management culture is one where workers feel confident to report, providers respond promptly, and participants are supported with dignity and respect.




































FAQs
Here is our frequently asked questions.