How to Support a Participant to Successfully Transition Into Care
Transitioning a participant into care is one of the most significant milestones in an NDIS participant's journey. Whether the individual is moving into Supported Independent Living (SIL), Specialist Disability Accommodation (SDA), Short Term Respite (STR), Individualised Living Options (ILO), or receiving in-home supports for the first time, the transition process sets the tone for the entire support relationship. A well-planned and thoughtfully executed transition builds trust, ensures safety, promotes comfort, and increases the likelihood of ongoing success.
Below is a detailed guide that explains how NDIS providers can create a smooth, respectful, and positive transition experience for participants and their families.
Transition Preparation
Preparation is the foundation of any successful transition. Before a single shift begins, providers must invest time in gathering information, understanding the participant’s unique needs, and developing appropriate support strategies.
A thorough preparation process involves reviewing all relevant documents such as assessments, medical reports, support plans, and the participant’s NDIS plan. Providers should make sure they understand the participant’s goals, daily routines, communication methods, cultural preferences, sensory needs, and any behavioural or emotional triggers. This information helps the provider develop a personalised support plan and an informed approach for risk management.
Preparation also includes identifying risks through a formal risk assessment. Providers should determine what support measures are required to keep the participant safe and comfortable and ensure that all workers are briefed and trained appropriately before commencing support.
Build Trust Through Transparent Communication
Having clear, consistent, and honest communication plays a crucial role in easing the participant’s anxiety and establishing a positive relationship. Transitioning into care can be overwhelming for both participants and family members, so transparency is essential.
Providers should offer detailed information about their services, including what the participant can expect each day, who will be supporting them, how communication will occur, and what responsibilities each party holds. This information should be delivered verbally and in writing to ensure clarity and accessibility.
It is also helpful to schedule time for participants or families to ask questions, raise concerns, or clarify expectations. When participants understand the process and feel heard, they experience less stress and greater confidence entering a new environment.
Involve the Participant in Every Step of the Process
The NDIS is built on the principles of choice and control, which means participants must be active contributors rather than passive recipients during the transition process. Involving participants in decision-making improves their sense of ownership and comfort.
Participants should be consulted about their preferred routines, worker preferences, cultural requirements, communication needs, meal choices, activities, and daily living preferences. Providers should place genuine importance to the participant’s voice and adapt the support plan wherever possible.
For participants with communication barriers, providers should use accessible and alternative communication methods. This may include visuals, easy-read information, translators, communication devices, or support from family members and advocates.
Conduct Meet-and-Greets and Compatibility Checks
One of the most effective ways to ease a participant into care is by organising meet-and-greets with workers and participants, before formal supports begin. These introductory meetings allow the participant to become familiar with the support workers, other participants and the environment which reduces anxiety and builds rapport.
Meet-and-greets also help the provider to determine whether workers and participants are compatible. Compatibility is especially important in settings such as SIL, where the participant will interact with workers frequently. These sessions give the participant a sense of control by allowing them to express preferences and provide feedback.
Families and carers should be invited to participate in the meet-and-greet process when appropriate, particularly when they play an important role in helping the participant feel safe.
Offer a Staged or Gradual Transition
Many participants benefit from a gradual, step-by-step transition rather than immediate full-time care. A staged transition allows participants to familiarise themselves with new environments, routines, and staff at a comfortable pace.
A staged transition might begin with a brief introductory visit, followed by a few hours of support, then a full day, and finally an overnight stay. This slower approach provides time to identify any concerns early, make necessary adjustments, and help the participant feel more secure.
This method is particularly important for individuals with high anxiety, sensory sensitivities, communication challenges, or complex support needs.
Create a Detailed and Individualised Transition Plan
An effective transition requires a structured and personalised transition plan that outlines how the participant will move into care and what supports will be provided during the process.
A strong transition plan should include:
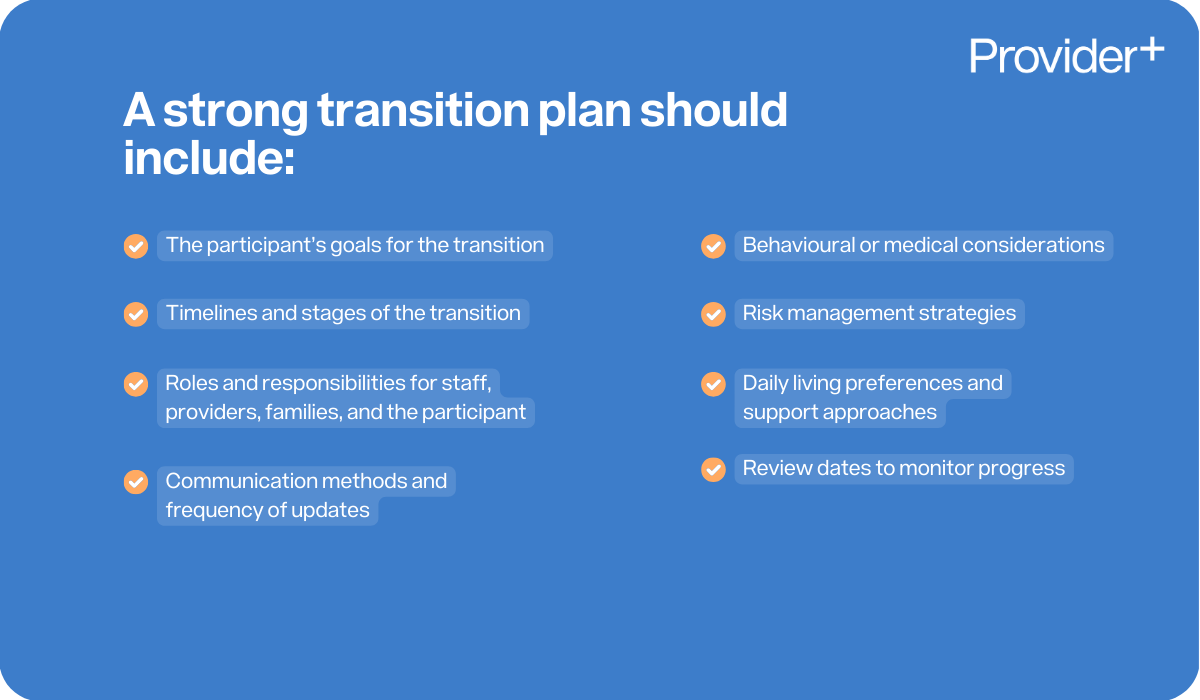
- The participant’s goals for the transition
- Timelines and stages of the transition
- Roles and responsibilities for staff, providers, families, and the participant
- Communication methods and frequency of updates
- Behavioural or medical considerations
- Risk management strategies
- Daily living preferences and support approaches
- Review dates to monitor progress
This documented plan ensures that every person involved understands their role, and it reduces the likelihood of confusion or miscommunication.
Encourage Active Participation from Family and Carers
Families, guardians, and primary carers often have the most in-depth understanding of the participant’s needs. Involving them in the transition process creates continuity, comfort, and reassurance for everyone involved.
Families can offer invaluable insights into routine, history, communication challenges, and personal preferences. Their presence during meet-and-greets, early stages of support, or planning meetings can help ease the participant’s nerves and provide additional context to the provider.
Providers should respect family knowledge, encourage collaboration, and maintain open, professional communication throughout the process.
Ensure Workers Are Properly Trained
Worker training is essential for a safe and successful transition. Workers should never begin care without completely understanding the participant’s profile and the support strategies required.
Training should include:
- Participant-specific needs and preferences
- Behaviour support plans (if applicable)
- Medical needs, including medication management
- Communication methods and any assistive technology
- Cultural, linguistic, or religious considerations
- Manual handling or mobility requirements
- Duty of care and safeguarding obligations
- Relevant NDIS Practice Standards and incident reporting procedures
When workers feel adequately prepared, they provide higher-quality support and build participant trust more effectively.
Maintain Thorough Documentation at Every Stage
Comprehensive documentation is vital for high-quality service delivery, audit compliance, and risk management. Providers should document every step of the transition, including assessments, communication logs, meeting notes, and updates.
Documentation should also include daily progress notes during the transition period, ensuring that staff are monitoring the participant’s wellbeing, comfort, and adjustment. This record becomes a valuable reference for improving the participant’s ongoing care.
Provide Ongoing Check-Ins and Continuous Support
A transition does not end once the participant has physically moved into care. Participants may still need emotional support, routine adjustments, or additional guidance as they settle in.
Providers should conduct regular check-ins with the participant, their family, and the support team to identify any issues early. Providers should also review the transition plan, assess whether goals are being met, and make necessary changes.
Ongoing support and proactive communication play an essential role in ensuring that the participant feels heard, supported, and understood long after the initial transition period.
Conclusion
A smooth transition into care is achieved through planning, communication, collaboration, and a strong commitment to person-centred support. When providers take the time to truly understand the participant and involve them and their family in every step of the process, the transition becomes a positive and empowering experience.
A successful transition lays the foundation for long-term trust, stability, progress, and wellbeing, ultimately creating a safe and supportive environment where participants can thrive.







.png)
