SIL Operational Guidelines for NDIS Providers 2025
Curious about NDIS Supported Independent Living (SIL)? We explain what SIL is, what it includes and doesn't include, and how you can ensure operational effectiveness and compliance, taking into consideration current registration requirements and planning for future registration requirements.
This NDIS Operational Guideline for Supported Independent Living (SIL) is designed to support providers with practical and up-to-date information on both compliance requirements and the operational aspects of managing a SIL home. It offers clear guidance on meeting the NDIS Practice Standards, and ensuring participant rights and safety to help providers deliver high-quality, person-centred supports in a compliant and sustainable way.
NDIS Supported Independent Living (SIL) Practice Standards

If you aren't aware the NDIS Commission is currently drafting NDIS Practice Standards that will focus solely on supported independent living (SIL). The Practice Standards will focus on quality and safety in shared accommodation with daily supports and will be co-designed with people with disability to ensure SIL supports are participant-centred, focused on human rights, respectful, understanding of privacy concerns and delivered by workers who have the right training.
What does this mean for providers?

The NDIS Practice Standards for Supported Independent Living (SIL) - currently in draft, signals a shift towards increased compliance requirements, with a stronger emphasis on accountability, participant safeguarding, and evidence-based service delivery. SIL providers will be expected to demonstrate more robust governance, clearer support planning processes, and improved oversight of day-to-day operations to ensure quality and consistency in participant outcomes.
Understanding NDIS Supported Independent Living (SIL)
Supported Independent Living (SIL) is a funded NDIS support designed to help people with disabilities live as independently as possible—whether in their own home or a shared living arrangement. It provides participants with the essential day-to-day assistance they need to build life skills, maintain a safe living environment, and lead a fulfilling life.
SIL funding covers support worker assistance tailored to each participant’s individual needs and goals. This includes help with personal care (such as bathing, grooming, and medication management), household tasks (like cooking, cleaning, and laundry), and support with daily routines. The intent is to reduce reliance over time and promote skill development in areas such as budgeting, decision-making, social interaction, and other daily living activities.
In addition to practical assistance, SIL offers important social and emotional benefits. Participants are supported to build connections, share responsibilities in a group setting if applicable, and participate in household and community life—fostering a sense of belonging and independence.
At its core, SIL is about supporting choice, control, and dignity—helping participants thrive in an environment that feels like home, while receiving the right level of support to meet their unique needs.

Pricing and Funding for Supported Independent Living (SIL)
Understanding the pricing and funding structure for Supported Independent Living is crucial for both participants and providers. SIL funding falls under the Core Supports budget of an NDIS plan and covers costs associated with daily living tasks in shared environments. The NDIS regulates the pricing structure to ensure consistency and fairness across services.
Participants do not pay for vacancy costs while the NDIA determines their SIL funding, minimising financial burdens during planning. SIL funding decisions are based on the participant’s needs and goals to ensure they receive the appropriate level of care.
While NDIS funding covers necessary supports for NDIS support independent living funding, participants remain accountable for their daily living expenses.
Exclusions in Supported Independent Living (SIL)
While Supported Independent Living offers extensive support, it is important to note what supported independent living funding does not cover. SIL funding is specifically designed to provide personal support rather than covering general living expenses.
Routine expenses like rent, groceries, and utility bills are not covered by SIL funding. Understanding this distinction helps participants and their families manage expectations and plan finances accordingly.
Expenses unrelated to the participant’s disability, such as vacation costs or personal budgeting assistance, are also excluded. Supports provided by other funding sources, such as health or justice systems, are also not covered under SIL.
Knowing these exclusions helps participants and providers focus on the supports SIL funding covers, optimising resource use.
Service Bookings and Compliance for Providers
Maintaining compliance with service bookings is essential for NDIS providers. Providers cannot claim for services rendered without established service bookings unless the participant’s plan is managed. Detailed records of service bookings must be maintained to adhere to NDIS standards and protect participant funding.
Adhering to approved funding ensures participants receive the services they are eligible for under their NDIS plan. This compliance underscores providers’ responsibility to operate within NDIS guidelines, ensuring the supports provided are consistent with the participant’s needs and goals.
Service Agreements
Key Inclusions for a SIL Service Agreement (Beyond a Standard NDIS Service Agreement)
A SIL (Supported Independent Living) service agreement should include additional, specific details beyond those in a standard NDIS agreement due to the complexity of shared living environments and the blending of support and daily living arrangements. Key elements to include are:

Including these items ensures transparency, safeguards participant rights, and supports a smooth, person-centred delivery of SIL supports.
- Board and Lodging Details
- Clear breakdown of what participants are expected to pay (e.g. rent, utilities, internet).
- What is and isn’t included (e.g. food preparation support vs. food costs, shared vs. personal hygiene items).
- Responsibilities for contributing to household expenses and how these are managed.
- Designated Living and Provider Working Spaces
- Acknowledgement of the participant's private and shared areas within the home.
- Agreement on the use of a designated workspace (if applicable), including whether the provider contributes to related costs (e.g. utilities, equipment).
- Shared Living Arrangements
- How supports will be delivered in a shared setting with other participants.
- Expectations around the use of common areas (e.g. cleaning schedules, shared responsibilities).
- Respect for private space, routines, and preferences of all residents.
- Integration with Other Service Providers
- If the home is a SDA dwelling (Specialist Disability Accommodation), outline roles, responsibilities, and communication protocols.
- Clarification of how the SIL provider will coordinate and communicate with external supports to avoid duplication or gaps.
- House Rules and Participant Rights
- Agreed expectations for living in a shared space (e.g. noise levels, visitors, safety protocols).
- How participants' rights, privacy, and choice will be upheld in the home environment.
SIL Roster of Care
SIL Roster of Care (RoC) – Key Considerations for Providers
Developing and managing a Roster of Care (RoC) is a critical component of operating a Supported Independent Living (SIL) service. It ensures that participant support needs are met safely, consistently, and in line with their NDIS plans. Providers must ensure the RoC accurately reflects the type, level, and complexity of supports delivered in the home, while also aligning with regulatory and funding requirements.
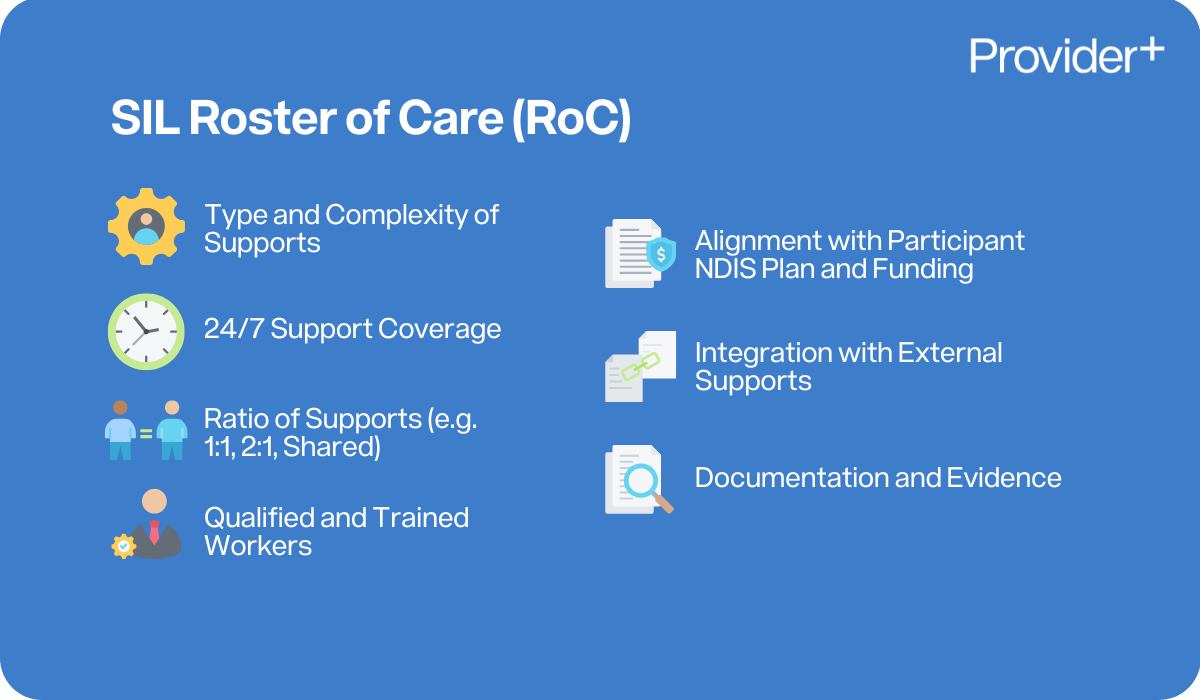
- Type and Complexity of Supports
- Clearly identify the individual needs of each participant, including personal care, behavioural supports, medical needs, and assistance with daily living.
- Ensure the roster reflects the complexity of supports, including shared and individualised time.
- 24/7 Support Coverage
- The RoC must demonstrate consistent 24/7 coverage, including active or sleepover shifts as required.
- Consider shift patterns, staff overlap for handovers, and breaks in compliance with the SCHADS Award and Fair Work requirements.
- Ratio of Supports (e.g. 1:1, 2:1, Shared)
- Clearly document the level of staffing support each participant requires at different times (e.g. 1:1 for personal care, 2:1 for behaviour management).
- Show how shared supports are allocated and managed amongst participants.
- Qualified and Trained Workers
- Ensure workers included in the RoC have the appropriate qualifications and training for the supports being delivered, which may include (not limited to):
- Medication administration
- Mealtime management
- Restrictive practices and positive behaviour support
- Include a plan for worker skill-matching based on participant needs (e.g. communication, manual handling, mental health).
- Ensure workers included in the RoC have the appropriate qualifications and training for the supports being delivered, which may include (not limited to):
- Alignment with Participant NDIS Plan and Funding
- The RoC must be consistent with the participant's NDIS funding allocation and goals.
- Ensure that the support hours and staffing levels proposed are reasonable and necessary and match the expectations of the NDIA.
- Integration with External Supports
- Account for times when participants are engaged in community participation or day programs, reducing overlap with SIL supports.
- Ensure coordination with external services (e.g. therapists, support coordination) is factored into the daily schedule.
- Documentation and Evidence
- Maintain up-to-date copies of the RoC and ensure changes are documented, justified, and communicated with participants and stakeholders.
- Ensure RoCs submitted to the NDIA for funding approval are clear, evidence-based, and participant-specific.
Price Guide / SCHADS Award
SIL Operations – Understanding the SCHADS Award and NDIS Price Guide Requirements
Supported Independent Living (SIL) providers must align their operational practices with both the NDIS Price Guide and the Social, Community, Home Care and Disability Services (SCHADS) Award. This ensures staff entitlements are met while maintaining compliance with pricing rules and workforce planning expectations. Key areas of focus include rosters, sleepover arrangements, workspace standards, and the treatment of staff entitlements such as breaks, overtime, and on-call duties.
Key Considerations for SIL Providers:
- Designated Workspaces for Staff
- Ensure a clearly designated work space and/or sleepover room for support workers that complies with WHS and privacy expectations.
- Workers should not deliver supports from participant bedrooms or shared participant spaces.
- If workers are expected to perform administrative tasks (e.g., incident reports), a suitable office or staff area should be available.
- Roster of Care Planning
- The Roster of Care must align with participant needs, funding approval, and SCHADS entitlements.
- Consider shift lengths, overlap for handovers, and ensuring adequate staffing for participants with high or complex needs.
- Sleepover Shifts (Active vs. Inactive)
- Clearly differentiate between active overnight shifts (where workers are expected to be awake and working) and inactive sleepover shifts (where workers are on premises and may rest, but can be called upon).
- Active overnight work is paid at standard hourly rates; inactive sleepovers are paid at the flat rate under SCHADS and must be claimed in accordance with the NDIS Price Guide.
- Recall to Duty – Night Interruptions
- Where workers on sleepover are woken and required to work, this constitutes a recall to duty and must be paid accordingly under the Award.
- Workers must track and record all night interruptions and ensure they are appropriately compensated, providers must have processes in place to accommodate this.
- On-Call Responsibilities
- On-call arrangements must comply with SCHADS conditions, including availability allowance and recall payments if the worker is required to respond.
- Ensure staff are trained in escalation protocols and have access to crisis response procedures.
- Span of Hours and Overtime
- Be mindful of SCHADS span of hours (generally 6 am–8 pm) and overtime penalties for work outside these hours.
- Roster planning must take into account fatigue management, maximum shift durations, and minimum rest periods between shifts.
- Right to Disconnect
- Under recent updates, workers have the right to disconnect when off-duty.
- Avoid contacting workers outside of their rostered hours unless on-call or in emergency situations.
- Continuity of Supports & Paid Breaks
- Providers must ensure adequate staff coverage during paid breaks to maintain continuous support, especially for participants requiring 24/7 supervision.
- Roster breaks in a way that doesn’t leave participants unattended or unsupported.
- Meal Planning – Workers and Participants
- Clarify whether workers will eat with participants or separately.
- If eating with participants: Consider participant consent, cultural sensitivities, and whether food is shared or prepared separately.
- If separate: Ensure there is a designated area for worker meals and storage.
- Establish clear boundaries between participant-funded groceries and worker personal food.
- Clarify whether workers will eat with participants or separately.
Service Delivery and Daily Operations / House Manager
SIL Operations and the Role of the House Manager – Key Responsibilities for Providers
The House Manager plays a central role in the successful and compliant operation of a Supported Independent Living (SIL) service. They are responsible for the day-to-day oversight of the home, ensuring supports are delivered in line with participant needs, NDIS requirements, and organisational policies. While support workers carry out daily tasks, the House Manager holds ultimate accountability for ensuring quality, safety, and continuity of care.

Key Responsibilities and Considerations:
- Liaison with the NDIA
- The House Manager, or nominated person with oversight of SIL properties, is responsible for liaising with the NDIA regarding Roster of Care submissions and approvals.
- Ensures alignment between funded supports, operational delivery, and participant needs.
- Staff Training and Mentoring
- Oversees the onboarding, training, and ongoing mentoring of support staff.
- Ensures all staff are trained in relevant areas, including medication, restrictive practices, manual handling, and participant-specific needs.
- Supervision and Workforce Management
- Provides regular supervision and performance monitoring of staff.
- Oversees workforce planning, rostering, and staff allocation based on participant support needs and house dynamics.
- Participant-Centred Service Delivery
- Ensures participant goals, rights, and preferences are prioritised in all aspects of support.
- Completes or oversees all required documentation, including care plans, incident reports, and progress notes.
- Acts as the main point of contact for families, guardians, and allied health professionals.
- Daily Operations Oversight
- While support workers carry out the day-to-day tasks, the House Manager maintains accountability for operational consistency, quality, and risk management.
- Coordinates property-related needs, including maintenance requests and WHS compliance.
- Shift Handover and Communication
- Maintains a formal handover process, including an up-to-date orientation booklet for each shift.
- Ensures clear and concise documentation is recorded and handed over between shifts for continuity of care.
- Information Management and Privacy
- Ensures compliance with privacy laws through secure, lockable storage areas for participant information, and medication.
- Trains staff in privacy obligations and information handling procedures.
- Ensures participant privacy and dignity is upheld.
- Incident Escalation and Reporting
- Responsible for timely and appropriate escalation of issues to senior management and/or external bodies.
- Manages reporting obligations to the NDIS Commission, including reportable incidents, complaints, and risk matters.
Medication / Mealtime Management
SIL Operations – Medication and Mealtime Management Supports
Effective medication and mealtime management in Supported Independent Living (SIL) is essential for participant safety, wellbeing, and dignity. Providers must implement clear procedures, ensure staff are appropriately trained, and align practices with NDIS Practice Standards. These responsibilities are especially important in shared living settings, where individual needs, preferences, and risks vary.
Medication Management – Key Requirements:
- Secure Storage
- All medications must be stored in a designated, lockable area that is only accessible to authorised workers.
- Consideration to where participants should not be restricted in their access to their medication.
- Separate storage for each participant's medication to avoid mix-ups, that is clearly identified.
- Webster Packs / Dispensary Systems
- Use of pharmacy-prepared Webster packs or similar systems to reduce risk and support accurate administration.
- Medication must be labelled clearly with the participant's name and dosage instructions.
- Participant Medication Plans
- Each participant must have an up-to-date medication management plan outlining their prescribed medications, administration requirements, potential side effects, and emergency instructions.
- Medication Administration and Record Keeping
- Workers must document every medication administered, missed, refused, or delayed dose in a medication administration record (MAR).
- Regular audits and reviews of records to ensure accuracy and compliance.
- Medication Incidents and Adverse Reactions
- Immediate reporting and documentation of any medication errors, missed doses, or adverse reactions.
- Follow organisational incident management procedures and escalate as required, including to the NDIS Commission if it's a reportable incident.
- First Aid Readiness
- First aid kits must be stocked and accessible at all times.
- Workers must know how to respond to medication-related emergencies and allergic reactions.
- Staff Training
- All workers involved in medication administration must receive accredited training in safe handling and administration.
- Regular refreshers and competency checks are required for workers.
Mealtime Management – Key Requirements:
- Meal Preparation and Storage
- Safe food handling procedures in place, including hygiene practices and correct food storage.
- Workers are trained in food safety and allergy awareness.
- Mealtime Management Plans
- Participants with swallowing difficulties or dietary requirements must have a documented mealtime management plan (e.g. texture-modified diets, supervision requirements).
- Plans should be developed in collaboration with health professionals (e.g. speech pathologists, dietitians).
- Allergies and Dietary Needs
- All known allergies and intolerances must be clearly documented and communicated to all workers.
- Prevent cross-contamination in shared kitchens.
- Participant Preferences and Menu Planning
- Respect individual food preferences, cultural requirements, and routines.
- Where multiple participants live in the home, include them in shared menu planning while still catering to individual choices and needs.
- Promote independence by supporting participants to participate in meal planning, shopping, and cooking where possible.
- Staff Training
- Staff must be trained in mealtime assistance, including choking prevention, safe swallowing techniques, and dietary compliance.
- Regularly review training against participants' changing needs.
Module 1
SIL Operations – Key Considerations for Module 1 Supports
Module 1 supports under the NDIS Practice Standards relate to the provision of high-intensity daily personal activities, which may include health-related tasks such as enteral feeding, catheter care, wound management, or other complex supports. Providers delivering these supports in a SIL setting must ensure workers are appropriately trained, participant safety is prioritised, and clinical oversight is in place where required.
Key Requirements and Considerations:
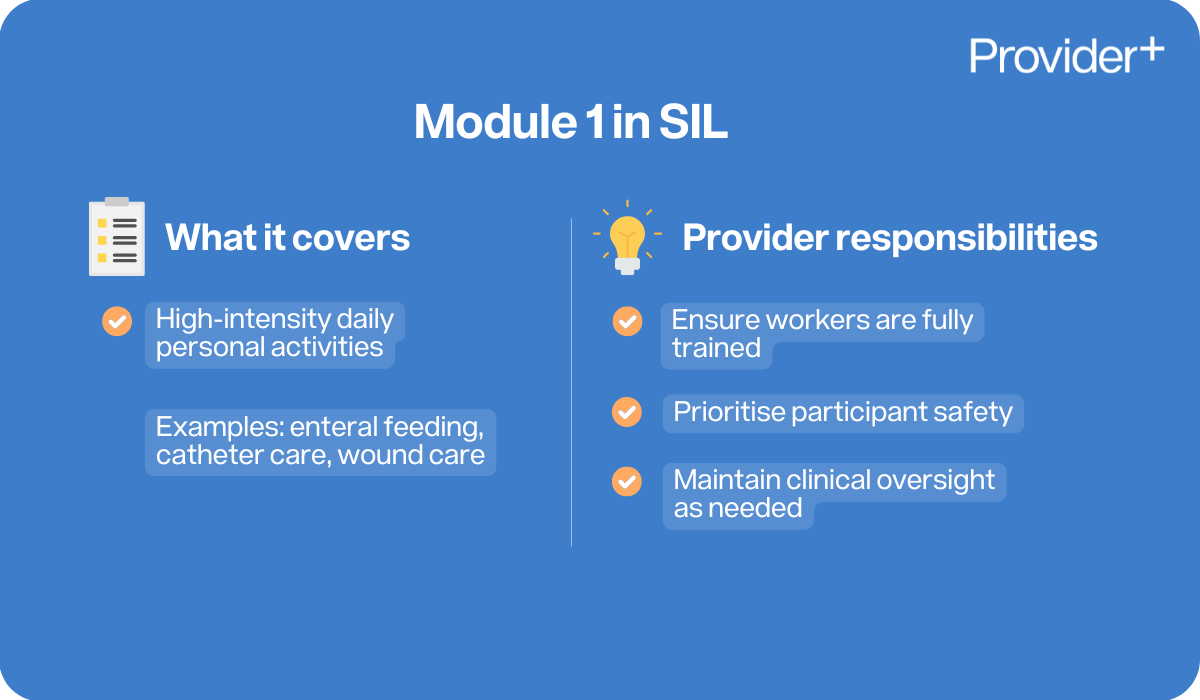
- Training and Competence of Workers
- All workers providing Module 1 supports must complete specific training relevant to the participant’s needs (e.g. PEG feeding, tracheostomy care).
- Workers must be deemed competent against the High Intensity Skills Descriptors.
- Training should be participant-specific and updated as needs evolve.
- Oversight by a Registered Nurse (RN)
- An RN may be required to oversee high-intensity supports, particularly where clinical judgement or monitoring is involved.
- Assess whether your participants’ needs require employing or contracting an RN for ongoing oversight, delegation, or complex case management.
- Ensure all delegation of tasks complies with relevant nursing standards and legislation.
- Management Plan
- Each participant receiving high-intensity supports must have a detailed support/health management plan in place.
- Plans must outline the tasks, risks, escalation procedures, worker training requirements, and monitoring protocols.
- Plans should be developed in consultation with healthcare professionals.
- Escalation Procedures for Health Concerns
- Clearly defined pathways for escalation in the event of a health incident or change in condition.
- Workers must be trained to recognise early warning signs and respond appropriately.
- Emergency contact information and protocols must be readily accessible.
- Client Confidentiality, Privacy, and Dignity
- Personal and health information must be stored securely in line with privacy legislation.
- Supports must be delivered respectfully, preserving dignity—particularly when managing personal or sensitive care tasks.
- Workers must maintain confidentiality at all times, including during handover and shift discussions.
- Designated Spaces for Clinical Activities
- Care tasks should be delivered in a private, clean, and designated area (e.g. participant bedroom or treatment room), not in communal or staff sleeping areas.
- Ensure the space is equipped with necessary PPE, clinical supplies, and safe disposal options (e.g. sharps containers).
- If a staff room is used for care coordination or documentation, it should remain separate from care delivery areas.
Implementing Restrictive Practices
SIL Operations – Implementing and Managing Restrictive Practices
Implementing Restrictive Practices in Supported Independent Living (SIL) environments is a highly regulated area of NDIS service delivery. Providers must ensure that any use of Restrictive Practices is clearly justified, authorised, reported, and aligned with the participant’s rights, dignity, and safety. Emphasis must always be placed on reducing and eliminating the use of Restrictive Practices over time.
Key Requirements and Considerations:
- Data Collection and Monthly Reporting
- Record all instances of regulated restrictive practices and submit monthly reports via the NDIS Commission's portal (through the Authorised Reporting Officer – ARO).
- Collect evidence such as behaviour incident reports, daily notes, staff observations, and environmental triggers to support positive behaviour planning and reviews.
- Maintain consistent and objective data to inform the Behaviour Support Plan (BSP).
- Worker Training and Competency
- All workers involved in implementing Restrictive Practices must be trained in:
- The types and definitions of restrictive practices
- Their legal responsibilities
- De-escalation techniques and alternatives to Restrictive Practices
- Reporting and documentation procedures
- Refresher training should be conducted regularly.
- All workers to receive training from the Behaviour Support Practitioner on the implementation and understanding of the Behaviour Support Plan.
- All workers involved in implementing Restrictive Practices must be trained in:
- Collaboration with Behaviour Support Practitioners (BSPs)
- Work closely with NDIS Behaviour Support Practitioners to ensure all Restrictive Practices are captured in the Behaviour Support Plan and are appropriate, authorised, and goal-oriented.
- Assist BSPs in collecting behaviour data and ensuring the plan is being followed correctly.
- Engaging Families, Guardians, and Other Providers
- Communicate openly with family members, guardians, and other relevant services (e.g. GPs, specialists, allied health, hospitals) to ensure a consistent and informed approach.
- Seek input for consent processes and ensure collaborative care planning.
- Respecting Participant Privacy and Dignity
- All Restrictive Practices must be implemented with the utmost respect for the participant’s privacy and dignity.
- Avoid any public or shaming practices and ensure care is delivered in private settings.
- Focus on Least Restrictive Option and Elimination
- Restrictive Practices should only be used as a last resort, for the shortest duration possible, and where all other alternatives have been tried and failed.
- Providers must work towards the gradual reduction and eventual elimination of Restrictive Practices wherever possible.
- Unregulated Restrictive Practices
- Providers must understand what constitutes an unregulated RP (e.g. environmental restraints not formally authorised) and recognise that these still require reporting and oversight.
- Develop internal processes for identifying, escalating, and addressing any unregulated or unauthorised practices.
- Emergency Services Collaboration and Crisis Response
- Establish clear protocols for involving emergency services during crisis situations.
- Provide scripts and behavioural escalation guides to help staff communicate effectively with police, ambulance, or mental health teams.
- Implement a Crisis Response Protocol, including clear decision pathways and contact points for escalation.
- Ensure on-call managers or behaviour specialists also have access to this protocol to support workers in real-time.
- Prevention of Violence, Abuse, Neglect, and Exploitation
- Ensure Restrictive Practices are never used punitively or as a means of convenience.
- Embed zero-tolerance policies and regularly review practices to identify any risk of abuse or neglect.
- Monitor for signs of excessive or inappropriate use of Restrictive Practices.
- Understanding What Is and Isn’t a Restrictive Practice
- Is a Restrictive Practice: Locking a door to prevent exit, using physical restraint, administering medication to control behaviour (chemical restraint), restricting access to personal items.
- Not a Restrictive Practice: Supportive prompts, redirection techniques, or safety measures applied equally to all residents (e.g. fire safety locks that can be opened freely).
- Train staff to differentiate between legitimate support strategies and actual Restrictive Practices to avoid under-reporting or misapplication.
- Roster of Care and Ratio of Support
- Ensure the Roster of Care (RoC) reflects the appropriate staffing ratio (e.g. 1:1, 2:1) required to safely implement any approved restrictive practices.
- Workforce planning must account for worker availability, training levels, and risk mitigation strategies.
- Adequate staffing must be maintained to provide safe, proactive support and minimise the need for restrictive interventions.
Reportable Incidents
SIL Operations – Key Considerations for Reportable Incidents
Supported Independent Living (SIL) providers must have robust systems in place for identifying, responding to, and reporting incidents—particularly those that are classified as reportable incidents under the NDIS Commission requirements. Failing to meet obligations can result in regulatory action, place participants at risk, and compromise service quality. Providers must ensure staff understand what constitutes a reportable incident and how to respond appropriately.
Key Requirements and Considerations:
- Understanding What Is a Reportable Incident
- Includes:
- Death of a participant
- Serious injury
- Abuse or neglect
- Sexual misconduct
- Unlawful use of a restrictive practice
- Misuse or unauthorised use of a participant’s funds
- All staff must be trained to identify and escalate these incidents immediately.
- Includes:
- Timeframes for Reporting
- Notify the NDIS Commission within 24 hours of becoming aware of the incident (for most incident types).
- For the unauthorised use of a restrictive practice, providers have up to 5 business days to notify, unless it caused harm, in which case it must be reported within 24 hours.
- Escalation internally must happen immediately—do not wait to confirm all details before initiating the notification process.
- Who Is Responsible for Reporting
- Providers must designate a responsible person (e.g. Compliance Officer, Service Manager) to submit reportable incidents to the NDIS Commission.
- All workers must know how and to whom they escalate incidents internally—usually to the House Manager or On-Call Manager.
- Escalation and Immediate Response
- Immediate action must be taken to ensure participant safety and provide any required support (e.g. medical care, police involvement, safeguarding).
- Activate internal escalation procedures and notify relevant parties (e.g. family, guardians, health professionals) as appropriate.
- Secure the environment and remove or address the source of risk, if possible.
- Investigation Process
- An internal investigation must be conducted to determine the cause and contributing factors of the incident.
- Collect statements, review documentation (e.g. rosters, incident logs), and interview involved parties where necessary.
- Maintain clear, objective, and factual records of findings and corrective actions taken.
- Risk Management and Continuous Improvement
- Conduct a risk assessment to prevent recurrence and identify service or system weaknesses.
- Update policies, procedures, and staff training based on incident learnings.
- Monitor trends through incident analysis and integrate findings into the provider’s continuous improvement plan.
Rights, Safeguarding and Compliance
SIL Operations – Participant Rights, Safeguarding & Provider Compliance
Operating a Supported Independent Living (SIL) service comes with increased responsibility due to the complex and often high-risk nature of shared living arrangements. Providers must maintain a strong focus on participant rights, safeguarding, and compliance—especially in light of regulatory requirements and the findings of the Disability Royal Commission. SIL is not just a service location—it is the participant’s home, and providers must treat it as such by promoting choice, control, and dignity at all times.
Key Requirements and Considerations:
- Upcoming Mandatory Registration for SIL Providers
- A requirement for all SIL providers to be registered with the NDIS Commission under the Assistance with Daily Living Tasks in a Group or Shared Living Arrangement registration group.
- Registration requires third-party certification audit and ongoing compliance with relevant NDIS Practice Standards.
- Compliance with NDIS Practice Standards
- All SIL providers must demonstrate compliance with the Core Module and relevant Supplementary Modules under the NDIS Practice Standards.
- This includes standards related to rights, governance, risk management, incident management, and provision of supports.
- New SIL-specific Practice Standards are expected to be released soon, with a stronger focus on safeguarding, home environments, and provider accountability.
- Increased Safeguarding Requirements
- The NDIS Commission is increasing its focus on participant safeguarding, following the recommendations of the Disability Royal Commission.
- Providers must have zero tolerance for violence, abuse, neglect, and exploitation, and must maintain a culture of transparency and immediate response to risk.
- SIL providers are expected to embed human rights principles into every aspect of support delivery.
- Participant Rights and Home Environment
- Remember: This is the participant’s home, not a workplace.
- Respect their right to privacy, dignity, autonomy, and cultural identity.
- Policies and practices should reinforce that participants are in control of their space, routines, and who enters their home.
- Participant Choice and Control
- Providers must actively involve participants in decision-making, including:
- Staffing preferences
- Daily routines
- Visitors and social interactions
- Menu planning and activities
- Respecting and enabling choice is essential to SIL compliance and participant wellbeing.
- Providers must actively involve participants in decision-making, including:
- Training and Workforce Development
- Workers in SIL require enhanced training, compared to those in community or group supports, due to:
- Higher complexity of needs
- Use of restrictive practices
- Medication administration
- 24/7 support context and risk escalation
- Ongoing competency checks and refresher training are essential.
- Workers in SIL require enhanced training, compared to those in community or group supports, due to:
- Vacancy Management and Participant Compatibility
- Managing vacancies must consider participant choice and compatibility.
- Good practice includes:
- Hosting meet and greet sessions, morning teas, or informal introductions
- Involving existing housemates in the process
- Offering trial stays (e.g. through Short-Term Accommodation/Respite)
- Using matching tools or preference questionnaires
- Document how the participant’s voice was included in the decision.
Emergency and Disaster Management
Emergency and Disaster Management in a SIL House – Key Inclusions
Effective emergency and disaster management is critical in a Supported Independent Living (SIL) setting to ensure participant safety and continuity of care. The following elements should be included and unique to each individual SIL property:
- Evacuation Plans and Procedures
- Site-specific evacuation maps and clearly documented procedures.
- Regularly reviewed and easily accessible evacuation plans.
- Procedures to assist participants with mobility, medical, or communication needs during evacuation.
- Training and Participation
- Evidence of staff training in emergency response protocols.
- Participant involvement in emergency drills and awareness sessions.
- Documentation of training completion and participant engagement.
- Evacuation Checklist and Grab Pack
- Quick-access checklist including:
- Secure access/exit (key locks considered in risk assessments)
- Personal Emergency Evacuation Plan (PEEP)
- Grab pack with essentials:
- Water, torch, spare batteries
- Mobile charger, long-life snacks
- Money, change of clothes
- First aid kit/PPE
- Copy of medication summary
- Spare car/house keys
- Quick-access checklist including:
- Risk Assessments and Equipment
- Individualised risk assessments covering mobility, equipment, medication, and communication needs.
- Backup power solutions (e.g. portable generators) for essential participant equipment.
- Identification of participants who may require additional support in an emergency.
- Alternative Accommodation Arrangements
- Pre-identified emergency accommodation options.
- Formal MOUs with alternative housing providers if relocation is required.
- Emergency Contact Information
- Up-to-date emergency contact details for all participants.
- Clear protocols for notifying family, guardians, and support coordinators.
- Coordination with Emergency Services
- Access to local emergency services contacts.
- Regular communication with emergency response teams where applicable.
A well-prepared emergency and disaster management plan ensures the safety, dignity, and continuity of care for all participants in a SIL setting.
Delivery Environment (the house)
Type of home - SDA, private rental, participant home, group home
House dynamics (preference, individual choice and control) - link this back to staffing as well - rostering considerations for risk mitigation and participant protection
SIL Delivery Environment – Key Considerations for the Home Setting
The physical environment of a Supported Independent Living (SIL) home plays a critical role in participant wellbeing, safety, and autonomy. Providers must ensure the home meets regulatory standards while balancing it as both a workplace for staff and a private, personal space for participants. The following elements should be addressed:
- Workplace Set-Up for Staff
- Clearly designated workspaces for staff, separate from participant living areas.
- Secure storage for documentation, medication, and work equipment.
- House Security and Access
- Secure entry/exit points with access systems appropriate to participant needs.
- Justification for use of locks or security devices where relevant (e.g. restrictive practices).
- CCTV use must comply with privacy laws and participant consent.
- Routine Inspections and Maintenance
- Property Risk Assessments are completed.
- Internal audits and regular checks (WHS, fire safety, electrical test and tag).
- Scheduled maintenance plans for household appliances and infrastructure.
- Cleanliness and Hygiene
- Cleaning routines clearly defined, including staff responsibilities and use of safe cleaning chemicals.
- Participants encouraged and supported to contribute to daily living tasks.
- Empowering Participants
- Opportunities for participants to develop independent living skills through shared responsibilities.
- Encourage active participation in meal prep, cleaning, and daily routines.
- Tailored support to build capability and independence at each participant's pace.
- Privacy, Dignity, and Personalisation
- Respect for personal boundaries and privacy in shared living environments.
- Each participant must have a private bedroom that is treated as their personal space.
- Staff must seek permission before entering a participant's bedroom and knock before entering, unless there is a safety concern.
- Bedroom doors should have locks (where safe and appropriate), and participants should control who accesses their room.
- Participants should be free to personalise their rooms with their choice of furniture, bedding, décor, and belongings.
- Rostered supports should ensure privacy is maintained during personal care routines, with minimal staff rotation where possible.
- All staff must be trained in respecting participant boundaries, personal routines, and rights to solitude.
- House Rules and Shared Living Dynamics
- Transparent house rules co-developed with participants.
- Clear expectations for shared space use, noise levels, and communal responsibilities.
- Strategies to manage interpersonal conflicts or differing lifestyles in shared homes.
- Visitor Management
- Participant choice and control over personal visitors, including overnight stays.
- When there are visitors, the provider will take into consideration the safety of other participants within the property to protect them from violence, abuse, neglect, exploitation or discrimination.
- Visitor registers and supervision protocols where necessary for safety.
- Risk assessments in place for visitor access in line with Service Agreement and tenancy arrangements.
- Visitor Management will take into consideration Privacy and Dignity needs of participants.
- Consideration for visitor sleepovers, impact on other participants and when a visitor is deemed a permanent tenant.
- Type of Home and Tenancy Arrangements
- Identify the nature of the property: SDA, private rental, group home, or participant-owned.
- Clearly define provider roles in maintaining or managing the property, if applicable.
- General Safety and PPE
- Availability of first aid kits, general PPE, and clear emergency response protocols.
- Staffing and House Dynamics
- Staff rostering aligned with participant preferences, behaviours, and risk mitigation strategies.
- Consideration of compatibility among participants and staff to promote a positive, respectful environment.
By addressing these areas, providers can ensure that the SIL home is a safe, respectful, and empowering environment that supports participant rights, independence, and quality of life.
Conflict of Interest
Conflict of Interest Management in SIL – Key Considerations
Managing conflict of interest (COI) in a Supported Independent Living (SIL) setting requires a tailored approach, distinct from standard support environments, due to the complexity of shared living, property management, and the intersection of personal, legal, and support relationships. Proper COI management ensures transparency, protects participant rights, and upholds the integrity of service delivery.
Key Elements to Include:
- Conflict of Interest Policy and Procedure
- A clear, written policy outlining how actual, perceived, or potential conflicts of interest are identified, disclosed, managed, and resolved.
- Specific procedures for managing conflicts related to shared living arrangements and property management.
- Conflict of Interest Register
- A maintained and regularly updated register that records any identified conflicts involving staff, management, or other stakeholders.
- Includes details of the conflict, assessment of risk, and actions taken to mitigate or manage it.
- Family and Personal Dynamics
- Consideration of complex family relationships, such as those involving estranged family members, informal carers, or family-provided supports.
- Ensuring participants are not placed in environments that could compromise their safety or independence due to family dynamics or personal relationships.
- Legal Orders and Considerations
- Processes in place to identify and manage legal complexities, such as:
- Guardianship and administration orders.
- Apprehended Violence Orders (AVOs).
- Custody or court-imposed living arrangements.
- Probation or parole conditions relevant to shared living or participant interaction.
- Processes in place to identify and manage legal complexities, such as:
- Multiple Providers (SIL/SDA/Other Services)
- Clear separation of roles when the SIL provider is also involved in SDA, support coordination, or other services to avoid undue influence or dual interests.
- Transparent agreements and participant choice upheld when engaging with multiple providers.
- Participant Choice and Control
- Ensuring conflicts of interest do not impact the participant's freedom to choose who delivers their supports, where they live, or who enters their home.
- Informed consent obtained in decisions involving co-tenants, support teams, or shared service arrangements.
- Participant Transparency
- Participants are kept fully informed of any potential or actual conflicts of interest that may affect their supports or living environment.
- Clear, accessible communication is used to explain how these conflicts are being managed, ensuring participants can make informed decisions.
- Risk Assessment and Documentation
- Regular risk assessments to evaluate how identified conflicts may impact participant safety or quality of care.
- Clear documentation of decisions and communications regarding conflict resolution, particularly where sensitive legal or family issues are involved.
- Training and Awareness
- Staff trained to recognise and report potential conflicts of interest.
- Emphasis on professional boundaries, especially where relationships may overlap.
By addressing these areas, SIL providers can ensure that conflict of interest is transparently managed, participants' rights are protected, and service delivery remains ethical, safe, and compliant with NDIS expectations.
Summary
In summary, understanding the operational requirements for Supported Independent Living (SIL) is essential for NDIS providers. SIL offers a pathway to greater independence, providing tailored support to manage daily activities and enhance the quality of life.
As we conclude this comprehensive guide, we hope it has provided valuable insights into the world of SIL. By understanding the various components, exclusions, and funding structures, participants and providers can navigate the complexities of SIL with confidence. Embrace the possibilities of independent living and take the first step towards a more empowered and fulfilling life.




































FAQs
Here is our frequently asked questions.